1 Background
Sleep complaints are extremely common in daily clinical practice. Altogether, sleep disorders affect more than 20% of the population 〚1, 2〛, have a chronic evolution and represent a high economical and social burden to Health and Social Assistance budgets.
Excessive sleepiness has important social impacts and accounts for many catastrophic accidents, as Chernobyl, the Challenger Space Shuttle, aeroplane accidents etc. Somnolence at the wheel is the third cause of traffic accidents, and accounts for 87% of the fatalities 〚3〛. One of the leading causes of hypersomnolence, the sleep apnoea syndrome, impacts on 2 to 4% of adults between 30 and 65 years 〚4〛.
The imperative need for efficient, rational, low cost strategies to cope with these disorders is clear. The first priority is to appropriately educate health care professionals throughout the community as how best to diagnose and treat these problems. However the long-term goal is to decrease health care expenses.
Treatment and diagnostic difficulties of General Practitioners (GP) associated with the above patients induce frequent consultation by different specialists, excessive and unnecessary medications, and useless laboratory tests. The high prevalence in the general population prevents a generalised care to all patients by dedicated experts, and contributes to the long waiting lists of many specialised centres.
Neurophysiological testing is an essential tool for diagnosis in sleep disorders. A large number of equipment is emerging on the market without any testing and validation; difficult problems of equipment compatibility are common and not solved in many laboratories.
Furthermore, neurophysiological testing does not usually consider the variability of demands of appropriate diagnosis, the versatility of equipment, the existence of automatic intelligent reporting and diagnosis, the ambulatory recordings and remote control of monitoring. Altogether these are essential steps for speeding up testing, while reducing costs.
The main objective of the study was to set-up and evaluate an experimental monitoring system for ambulatory sleep medicine.
2 Material and methods
2.1 Sleep technology: evaluation of sleep monitoring system
An ambulatory monitor manufactured by CIDELEC (49130 Sainte-Gemmes-sur-Loire, France) has been tested. It includes two devices: CID 102 and CID 108 (Fig. 1).
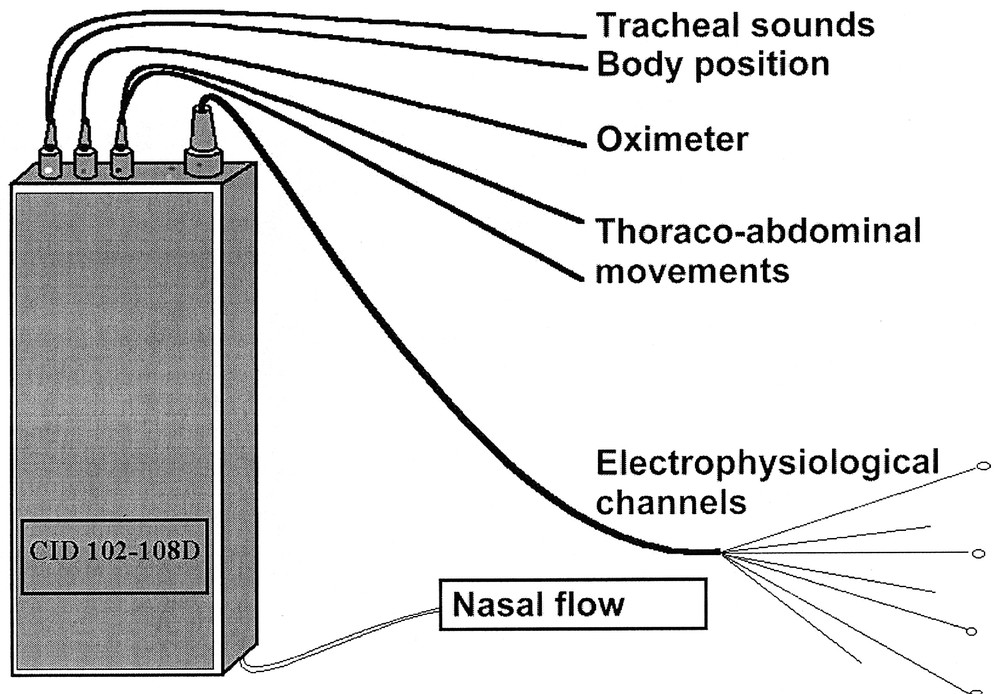
Schematic diagram of the CIDs 102 and 108 with the channels recorded (see abbreviations in the text).
The CID 102 records the following channels: tracheal sounds with a microphone taped on the lateral side of the neck, nasal flow with a cannula linked to a pressure transducer, oxygen saturation by digital oximetry, heart rate through the pulse oximetry signal, thoracic and abdominal perimeters with piezo-electric sensors, body position by a mercury sensor. These channels are recorded at 16 Hz.
The CID 108 records neurophysiological channels at 128 Hz: two EEG (A1-C2, A2-C1) according to the 10–20 international system, two electrooculograms (EOG), one submental electromyogram (EMG) and one tibial EMG.
Data are recorded in a solid-state memory and transferred on a PC at the end of recording for further analysis or sent by Internet using FTP to a reference centre. Sleep stages have been visually determined on the computer screen by trained physicians according to the conventional criteria 〚5〛. Breathing abnormalities detected by the automatic analysis have been validated by the physician to document the presence of apnoea, hypopnoea and flow limitations according to usual criteria 〚6〛. Namely apnoea was defined on the nasal flow signal when amplitude decreased to less than 10% of the preceding 5 min. Hypopnoea were scored when this amplitude was decreased between 10 and 70% in association with a fall greater or equal to 3% in oximetry. Flow limitation was scored when the fall in amplitude was not associated with a fall in oximetry. Only periods with validated (not artefacted) oximetry have been considered for reporting the results.
2.2 Patients
Twenty-five patients (among whom five women) have been recorded. They were suspected of sleep apnoea on the association of daytime sleepiness as measured by an Epworth scale above 11 〚7〛 and habitual loud snoring. Their mean age (range) was: 52 (45–72) years and body mass index 28 (26–35) kg m–2.
Fifteen patients had a set-up at home by a health care organisation (ADEP, Suresnes, France), which included both CIDs 102 and 108. Ten patients had a CID 102 recording with a set-up at the hospital and a recording at their home.
3 Results
3.1 Quality of signals
Two recordings over 15 (15%) full polysomnographies had a failure of neurophysiological recording, but the respiratory recordings remained usable.
No failure was experienced in the CID 102 respiratory recordings, although in some patients 10 to 15% of tracings had oximetric artefacts.
Total sleep time were 345 ± 128 min (mean ± SD) and sleep stage repartition was 65 ± 12% of stages I et II, 15 ± 8% of stages 3 et 4 and 16 ± 9% of REM sleep.
3.2 Diagnosis
Seventeen over 25 patients have been diagnosed as sleep apnoea syndrome with AHI index > 15 h–1.
Three had an upper airways resistance syndrome 〚8〛 with arousal associated flow limitations.
Four had simple snoring without respiratory event and one had myoclonia associated with snoring.
4 Discussion
Sleep recordings have several specificities: they last several hours therefore they require special sensors and often duplicate signals to maintain readable overall tracings. The techniques used must not modify the sleep structure that they are designed to record. Home recording is desirable to obtain a more natural sleep than in the laboratory.
Few types of equipment have been tested so far for home recording 〚9, 10〛. The CIDELEC system has only been studied in a hospital setting but not in home recordings 〚11〛. Recently one study has compared home versus hospital recordings and shown a good sensitivity of such recordings for the diagnosis of sleep disordered breathing together with a lower economical cost 〚10〛. The failure rate was: 20% and the acceptability by the patients was the same at home as in the hospital.
Failure rate is a problem but is more often related to neurophysiological signals than to respiratory signals. This may be due to the difficulty to set-up EEG electrodes by insufficiently trained technician but also to the conditions of home recordings where a permanent check of the signals is impossible 〚12〛.
The results given by the analysis of the usually remaining respiratory signals may allow a proper diagnosis 〚13〛 but this is controversial as the determination of actual sleep time is necessary to compute the apnoea–hypopnoea index and arousals are so far best determined by EEG analysis although new methods are appearing 〚14〛. The sensitivity of respiratory recording is too low for screening sleep respiratory disorders but may be sufficient in patient with high pre-test probability of disease and allow more resources for full polysomnography in patients with negative screening tests 〚15〛.
This system could be implemented in a healthcare network aimed at providing a better care by involving the general practicians to the diagnosis and follow-up of sleep patients. This network is planned according to the scheme displayed in Fig. 2. Three levels of care are in charge of the patient: level 1 is the GP who is trained by the network to screen for sleep disorders using self-administered questionnaire and clinical rules. When necessary the GP can contact level 2, managed by specialists for specific etiologies (psychiatrist, ENT, endocrinologist...) or access to specialised diagnostic tools through the regulation of the medical coordinator. Level 3 of access is reserved for difficult diagnosis requiring specialised techniques or uncommon therapeutic interventions.
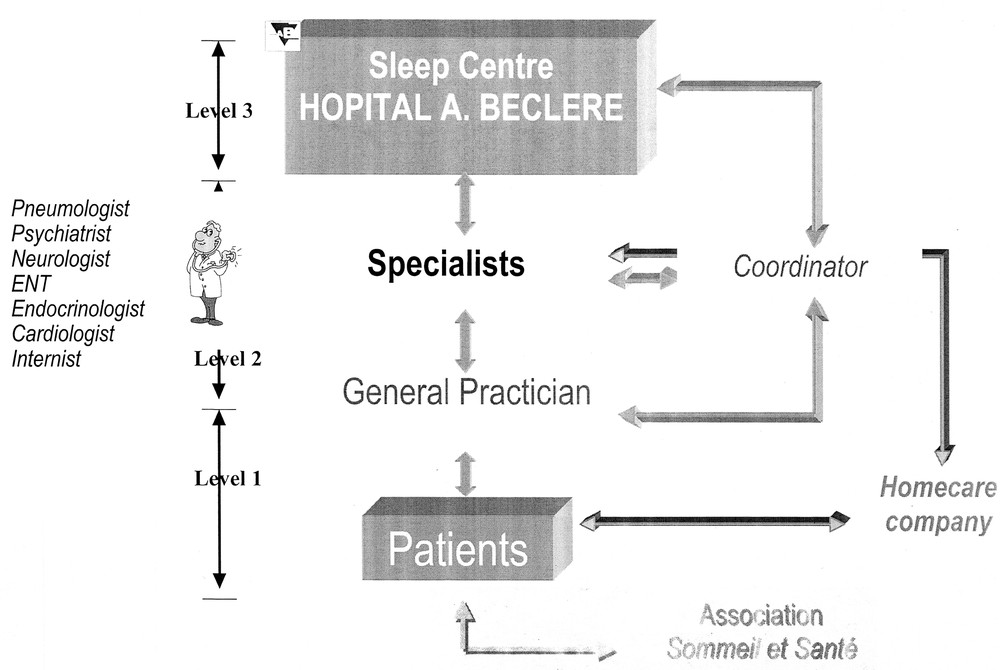
Diagram of the sleep health care network.
All actors of the network will be linked by a teletransmission system through Internet to a common patient file with secured access.
5 Conclusion
The ambulatory monitoring system fits into the scheme of a sleep healthcare network and should allow a better care for the sleep respiratory disorders.
Acknowledgements
This research has been supported by the programme ‘ACI Télémédecine et technologies pour la santé’ No. 157/99.
Version abrégée
1 Introduction
La prévalence des troubles du sommeil dans la population générale est élevée : 20% d’adultes souffrent d’insomnie, 10% sont hypersomnolents le jour, 2 à 4% ont des troubles respiratoires du sommeil. La disponibilité insuffisante des centres de sommeil impose la recherche de techniques alternatives d’enregistrement du sommeil. L’enregistrement ambulatoire présente l’avantage d’étudier le sommeil dans l’environnement naturel du patient, en faisant l’économie d’une hospitalisation. Néanmoins, les moniteurs actuels ne sont pas tous adaptés à l’enregistrement des paramètres physiologiques sans surveillance.
2 Objectifs
L’objectif de cette étude réside dans l’évaluation d’un enregistreur ambulatoire pour les troubles du sommeil et de son intégration dans un réseau de soins.
3 Méthodes
Un moniteur ambulatoire de la société Cidelec (49130 Sainte-Gemmes-sur-Loire), CID 102 et 108 a été évalué. Les voies enregistrées comportent : les sons trachéaux (microphone collé sur la peau au niveau du cou), le flux nasal par canule reliée à un capteur de pression, la saturation en O2 (oxymètre digital), la fréquence cardiaque, les efforts thoraciques et abdominaux (sangles piézo-électriques), la position corporelle (CID 102) et des voies neuro-physiologiques échantillonnées à 128 Hz (2 EEG, 1 EMG, 2 EOG) par le CID 108.
4 Patients
Quinze patients ont subi un branchement (CID 102 + 108) à domicile par une association de soins à domicile (ADEP). Dix patients ont été branchés à l’hôpital et ont subi un enregistrement à domicile (CID 102).
Ils étaient suspects de ronflement ou de syndrome d’apnées du sommeil sur l’association ronflement–hypersomnolence diurne.
5 Résultats
Les stades de sommeil ont été déterminés visuellement par lecture des signaux neurophysiologiques. Les anomalies respiratoires détectées par l’analyse automatique ont été validées par un médecin formé à la pathologie du sommeil.
Les échecs techniques ont été de 2/15 avec l’enregistrement complet à domicile (CID 102 + 108). Il n’y a pas eu d’échec pour les tracés respiratoires (CID 102).
6 Intégration en réseau
Un réseau expérimental de médecine du sommeil est en cours de mise en place sur le département 92 avec le soutien de l’ARH (Agence régionale de l'hospitalisation) et de l’AP–HP. Il comportera des actions de formation des médecins généralistes, des liaisons de télétransmission avec les spécialistes (psychiatres, neurologues, ORL, pneumologues...) et les centres de sommeil. Un médecin coordonnera l’ensemble du réseau.
7 Conclusion
L’enregistrement ambulatoire tient une place importante dans le fonctionnement de ce réseau, les données compressées des enregistrements pouvant être transmises par connexion Internet sécurisée.