1 Introduction
The awareness of stone composition and a metabolic evaluation grants a better understanding of urolithiasis prognosis, recurrence risks, as well as improvements in their medical and surgical management. For instance, stone free rates regarding shockwave lithotripsy (SWL) rely on the stone burden and composition, with calcium oxalate monohydrate stones being the hardest and with less stone free rates [1,2]. Also within the same type of stone composition, the efficacy of different treatments can differ. Such is the case of cystine stones regarding its treatment with SWL or retrograde intrarenal surgery (RIRS) [3].
Flexible ureterorenoscopy (F-URS) has had significant advancements in the matter of technology and image quality during the last two decades. Today, more and more urologists have integrated this technique in their daily practice (Fig. 1).

Digital flexible ureterorenoscopy with an endoscopic high-quality vision of a kidney stone.
The literature confirming the effectiveness and safety of F-URS in the treatment of renal stones is more and more abundant [4]. The smaller size, durability and maneuverability of the ureterorenoscope are continuing to evolve thus facilitating the operator to increase the effectiveness of this treatment. One of the limitations of F-URS is that the stone analysis is often performed only on a limited number of small fragments retrieved, without any information considering the location of these fragments within the stone. Considering that much of the stones have mixed compositions [5], important details of the stone composition could be missed if there are no more characteristics transmitted with the stone fragment.
In the near future, we hope that macroscopic stone evaluation during F-URS through the image quality could aid the assessment of stone composition, morphology and metabolic evaluation. The aim of the manuscript is to describe the advances in endourology and F-URS, and to discuss what is known on endoscopy per-operative evaluation of stones.
2 Advances in endourology and flexible ureterorenoscopy
2.1 Ureterorenoscopes
Bagley et al. described the first flexible ureterorenoscope in 1983. It consisted of a flexible tip endoscope with 160–90 degrees of maximum deflection [6]. Since that time, the technology advancement of the F-URS has progressed at a remarkable pace (Fig. 2).

Contemporary fiber optic and digital flexible ureterorenoscopes.
2.1.1 Old generation flexible ureterorenoscope
Standard ureterorenoscopes (old generation) are 70 cm long with a disk-shaped distal extremity of 7.4 F, which progressively grows until 9 F on its proximal site. A working channel of 3.6 F will allow the use of instruments through it until 3.2 F, including laser fibers and nitinol baskets for stone retrieval. Two or three fiber optic bundles are responsible for the illumination and for image transmission. The angle of the view of this ureterorenoscope is 0° with a field of view of 90°.
These old generation flexible ureterorenoscopes have an active deflection of 180° downward and upward and were used until 2001, when improvement in image quality, handling ergonomics and more deflexion degrees were achieved for the new generation ureterorenoscopes.
2.1.2 New generation flexible ureterorenoscope
One of the advantages of new generation ureterorenoscopes is the possibility of achieving an active deflection up to 270° (Fig. 3). The image quality has little variations between companies, which depends on the number of fiber optic bundles used for illumination and image transmission.

Active 270-degree deflection during an F-URS of a complex lower renal pole in a horseshoe kidney patient.
These ureterorenoscopy images have a “honeycomb” effect, which would decrease as the number of fiber optic bundles increases. Nevertheless, the more and smaller the fiber optic bundles are, the more prone to damage they will be.
In order to increase the strength of the flexible ureterorenoscopes, as well as to facilitate the renal cavity access and endoscope control, the newest endoscopes have become more rigid or better-called “semi-flexible ureterorenoscopes” (Fig. 4). Studies are still waiting to demonstrate if there is an interest or improvement during the F-URS when using this type of ureteroscope.

“Semi-flexible” ureterorenoscopes' rigidity (top) compared to conventional flexible ureterorenoscopes (bottom).
Despite the technological progression in these ureterorenoscopes, they remain fragile. The mean number of cases performed with a fiber optic ureterorenoscope before their repair ranged between 3.2–14.4 procedures [7], while that with digital endoscopes ranged from 21–135 procedures [8]. In spite of this, some authors have reported up to 100 cases and more than 74 h performance with fiber optic endoscopes and 107 h for digital endoscopes [9,10].
2.1.3 New digital generation flexible ureterorenoscope
Since 2006, the digital technology has represented the next step in the development of endoscopy with a distal sensor. Many studies have showed that a better image quality provides a higher precision for diagnosis, treatment and a shorter procedure time. The digital ureterorenoscopes use a Complementary Metal Oxide Semiconductor (CMOS) or charge-coupled device (CCD) imaging sensor as the digital camera and a light-emitting diode (LED) as the light source.
The principal disadvantage with the digital generation is the distal tip diameters that are slightly greater than those of the equivalent standard fiber optic ureterorenoscope. This digital generation is now considered the gold standard for image quality (Fig. 5).

Comparison between fiber optic and digital flexible ureterorenoscopy image quality in stones (left) and ureteropelvic junction stenosis (right).
2.1.4 Disposable flexible ureterorenoscope
In 2009, the PolyScope by Lumenis became available. This is a disposable, modular flexible ureterorenoscope with a 70 cm working length and a distal tip size of 9.6 F. It has a single-side active deflection of 180°, and the working channel is 3.6 F. Currently, more studies are needed to demonstrate the efficiency and cost-effectiveness of this device, which is more difficult to manipulate than the usual flexible ureterorenoscopes.
2.2 Irrigation
Irrigation during F-URS is essential in order to work in the urinary tract. It allows renal cavity dilation and better visibility by cleaning the urinary tract. Special attention should be paid regarding the irrigation fluid pressure, in order to avoid over increase in intrarenal pressure (Fig. 6).

Continuous irrigation with a manual hand pump to increase the irrigation while needed (TraxerFlow, Rocamed).
There are several irrigation dispositives, which allow working with a continuous fluid irrigation, and when needed, the irrigation can be transitorily increased to offer better visibility with the manual hand pump. Moreover, a ureteral access sheath (UAS) has been developed in order to reduce the intrarenal pressure during F-URS.
2.3 Ureteral access sheath (UAS)
The UAS consists of a device with two hydrophilic pieces: the sheath and an internal dilator (Fig. 7). It is inserted over a guidewire under fluoroscopic guidance (Fig. 8). The use of the UAS has been proven to help during F-URS since it allows us to engage easily the ureter, to perform more stone retrieval movements, it dilates the ureter, improves vision by facilitating the outflow of irrigation fluid, lowers the intrarenal pressure and also protects the ureterorenoscope while giving it more stability which enhances the control of the scope in the renal cavities. Besides, the UAS may reduce the operating time and costs [11]. A UAS is not mandatory during F-URS and its use is according to the surgeon’s preference.

Ureteral access sheath (ReTrace, Coloplast). The external sheath appears in orange and the internal dilator in gray.

Insertion of a UAS over a guidewire under fluoroscopic guidance.
2.4 Lithotripter
The lithotripter of choice in F-URS is the Holmium-Yttrium-Aluminium-Garnet crystal (Holmium-YAG) laser. This laser wavelength is well absorbed in water (1 mm in depth) with tissue penetration of only 0.5 mm (Figs. 9)[12].

A Holmium-YAG 30W laser lithotripter (Rocamed).
Holmium-YAG laser setting can be settled for stone fragmentation using high energy (1–2 J) and low frequency (3–5 Hz) or stone dusting using low energy (0.2–0.5 J) and high frequency (10–20 Hz). Stone fragmentation would allow the removal of small stone fragments, which could be subsequently analyzed (Fig. 10). Stone dusting on the other hand would create a lower rate of significant fragments, which would be eventually expelled by the patient (Fig. 11).

Small stone fragment retrieval using a tipless nitinol basket.

Kidney stone dusting. Initial aspect (left) and final results (right).
3 Discussion
Pak et al. in 1980 published that the metabolic evaluation for urolithiasis should be simple, economically viable and should provide enough information towards a selective and rational therapy [13]. Today, most of the first time stone formers would have a basic metabolic evaluation and a stone composition analysis, since their recurrence risk is 50% within the next 10 years [14].
Despite this, in some scenarios stone composition analysis is not available leaving only the option of a metabolic analysis to determine the type of stone. Although some metabolic disorders are associated with stone types, such as metabolic syndrome and uric acid stones [15], it still remains unknown whether these findings could strongly predict the stone type. Xu et al. collected data from 1164 patients who were admitted in a urology department and were assessed for blood serum electrolyte analysis, but no differences were found between stone former and non-stone former patients [16]. Urinalysis on the other hand has been a widely used tool for metabolic evaluation of stone formers, but its efficacy remains controversial. Moreira et al confirmed the role of 24-h urinalysis in predicting the stone types, however the accuracy of 24-h urinalysis alone was only 64% [17].
Therefore, in some cases a combination of metabolic assessment and 24-h urinalysis may not be enough for predicting the stone type. Thus a combination assessment of metabolic, urinalysis, radiological and advanced techniques in endourology may improve the accuracy in determining the morpho-constitutional stone analysis of patients.
With technological advancements in image quality in F-URS, such as the incorporation of an optical chip like CMOS or CCD along with a distal LED light and image processing capabilities, urologists may now be able to define the macroscopic characteristics of urolithiasis (Fig. 12). These improvements on the last generation of digital F-URS are now very useful to ensure a diagnosis and even to spare time during stone photovaporization [10].

Endoscopic morpho-constitutional aspects of the most frequent types of uinary stones.
The macroscopic characteristics of stones include their size assessment, stone colors and surface variations, as well as the outer and inner stone layer characteristics while performing lithotripsy, stone hardness and even the scent during lithotripsy as happens with cystine stones.
When comparing known diameters of safety guidewires, laser fibers and UAS with the stones, urologists can accurately perform stone size assessment [18]. Despite there are no high-level evidence studies in the literature, we believe that the macroscopic aspect and color of stones may raise the likehood of their composition (Fig. 13). For instance, calcium oxalate monohydrate may appear in dark colors and rounded shapes, while calcium oxalate dihydrate and cystine stones emerge in yellow/golden “star” shapes and uric acid stones in yellow rounded shapes (Fig. 14).
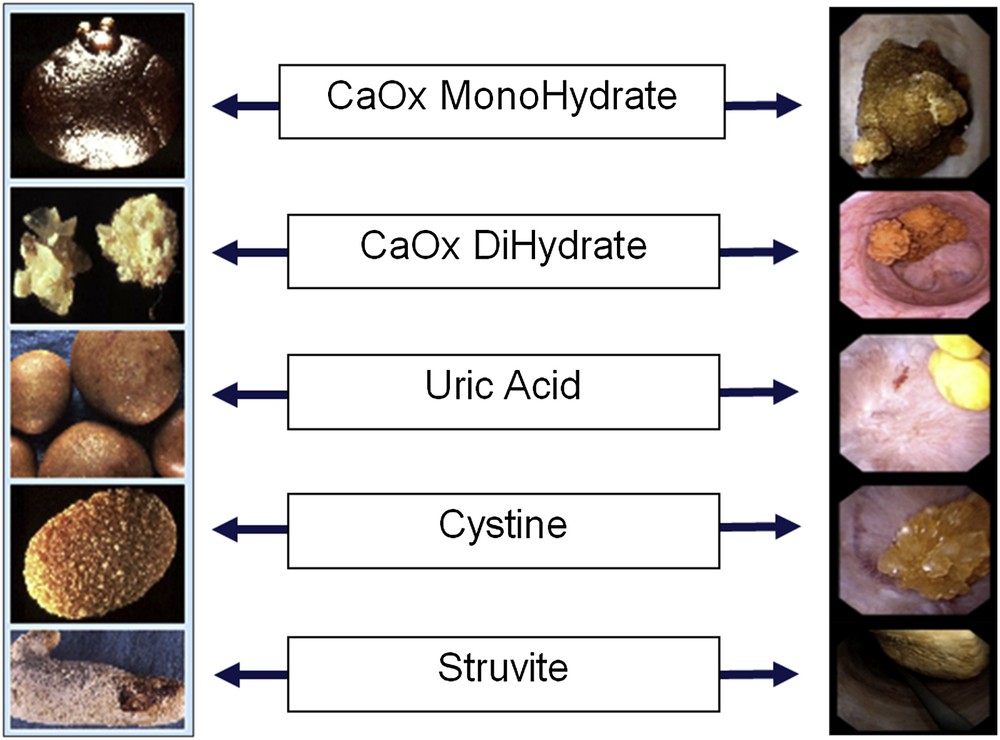
Comparative images of macroscopic and endoscopic “in situ” morpho-constitutional aspects of the 5 commonest stone types.

“In situ” morpho-constitutional analysis of calcium oxalate dihydrate (left) and uric acid (right) stones, endoscopic and macroscopic views.
As previously mentioned, the outer and inner stone layers might have a different composition and macroscopic aspect during F-URS, but out of a 15 mm kidney stone only a small fragment is analyzed which could bias the result of stone analysis. Moreover, laser lithotripsy may raise the suspicions of different stone compositions while performing it, since the core and outer layers of stones may be harder or softer than each other regarding their composition (Figs. 15 and 16).

Macroscopic differences of the outer and inner layers within the same stone.
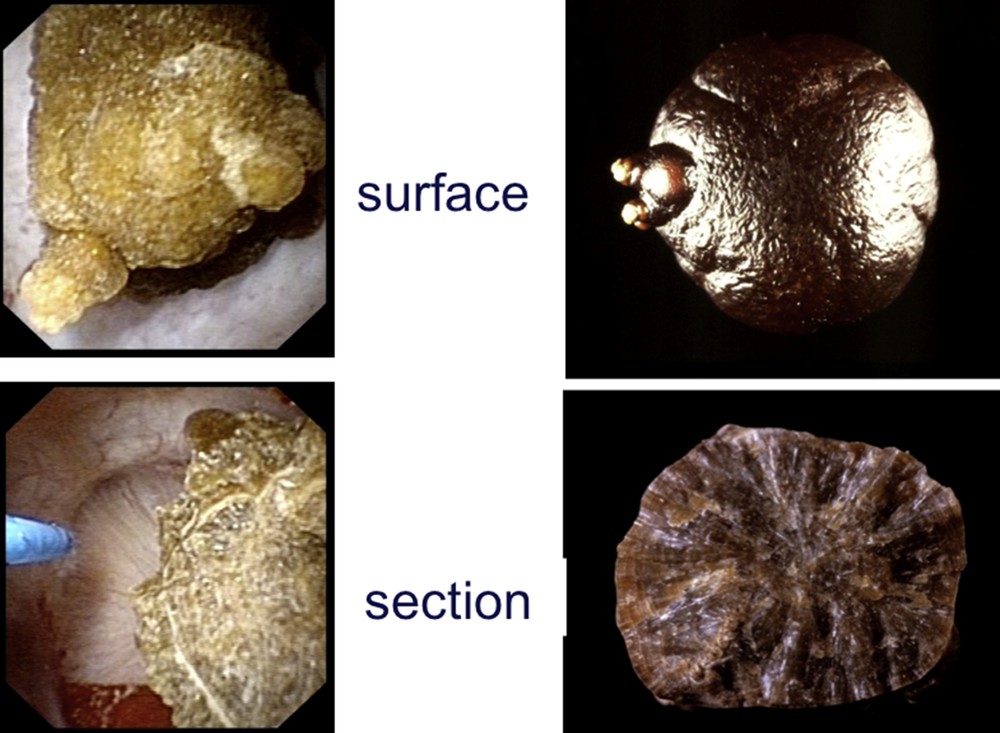
Endoscopic and macroscopic views of the surface and sections of a calcium oxalate monohydrate stone.
To date, there is no scientific evidence regarding the advantages of endoscopic stone morpho-constitutional evaluation. However, further studies analyzing the accuracy of the endoscopic stone evaluation are needed to better know if it might improve the final description of the morpho-constitutional stone type. This interest of the technology advancement could counterbalance the fact that F-URS most of the time allows to send only a small part of the stone burden for the analysis.
4 Conclusion
Technological advancements in the field of F-URS may be an important tool in the assessment of stone morphology and composition. It is very important for urologists to know the development in this field and the equipment available to accommodate them during all the procedures.
New prospective and randomized trials are needed in order to evaluate the role of endoscopic evaluation or video during F-URS in determining the morpho-constitutional analysis of the stone that could also be associated with specific metabolic anomalies [19].
Disclosure statement
One of the authors is a consultant for Coloplast, Rocamed, Olympus and AMS.
No competing financial interest exists.
Acknowledgments
None.


